Novel Protocol to Rapidly Diagnose and Treat Central Retinal Artery Occlusion
Ophthalmologists at New York Eye and Ear Infirmary of Mount Sinai (NYEE) have created a novel protocol to rapidly diagnose eye stroke and expedite care to prevent irreversible vision loss.
Their study, published in Ophthalmology, describes using high-resolution retinal imaging in the emergency room, along with rapid remote consultation to confirm diagnosis and expedite care, improving outcomes for eye stroke patients and preserving vision.
“The protocol implements highly sensitive retinal imaging at the patient’s point of entry into the medical system, reducing the need for onsite ophthalmology consults, which are often not immediately available,” says corresponding author Richard B. Rosen, MD, Chief of the Retina Service for the Mount Sinai Health System. “Seamless cooperation and coordination between the subspecialty teams of stroke neurologists, retinal specialists, and interventional radiologists is the key to rapid triage of these emergency patients. This model can easily be implemented anywhere in the country where a stroke team is available, The semi-automated OCT camera and remote consult team can expedite diagnosis for these time-sensitive eye emergencies.”
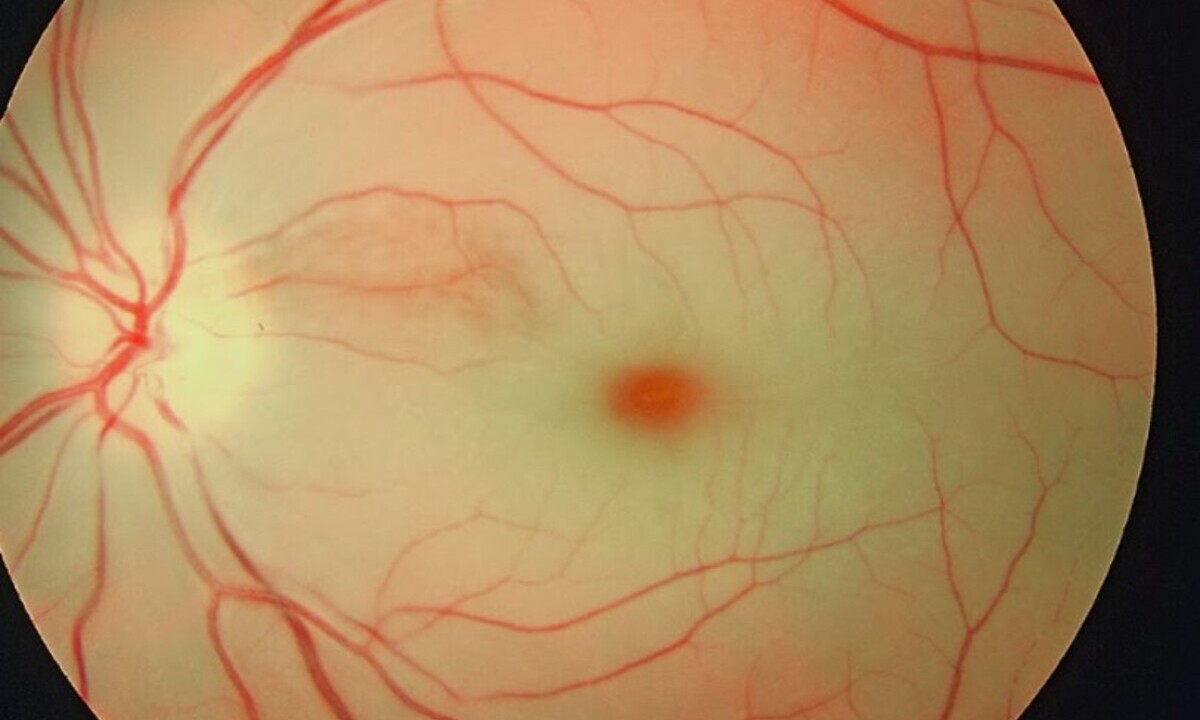
Painless, sudden vision loss in one eye may be a sign of an eye stroke, also known as central retinal artery occlusion. It happens when the main artery that supplies blood to the retina is blocked, typically by a clot, depriving the retina of oxygen. The retinal nerve cells that allow you to see die within hours unless blood flow is restored. The clot needs to be dissolved as soon as possible, ideally within 6 to 12 hours of losing vision, or it will lead to permanent vision loss.
To expedite care, Mount Sinai’s Department of Ophthalmology launched an Eye Stroke Service and developed a treatment protocol for patients. High-tech eye imaging devices using optical coherence tomography (OCT) were placed in three hospitals within the Mount Sinai Health System that have large emergency rooms and stroke teams. OCT diagnostic imaging, pioneered at NYEE, is a non-invasive way to detect microscopic changes in the retina within minutes of a blockage, enabling rapid diagnosis for accurate treatment.
When a patient arrives at the emergency room with a possible eye stroke, the stroke service is urgently called to evaluate the patient and do the scan. They electronically send the images to remote on-call retinal specialists who can make an instant diagnosis. If the retinal specialists confirm an eye stroke diagnosis, the vascular interventional neuroradiologists can dissolve the clot with an infusion of tissue plasminogen activator (tPA)—a clot-dissolving drug—into the blocked ophthalmic artery.
Researchers analyzed 59 patients who went through the protocol on the Eye Stroke Service during the first 18 months since it launched. The average time to treatment after the patients arrived at the hospital was roughly two and a half hours. Patients were treated, on average, about nine hours from the onset of symptoms, which included the time the patients took to come to the hospital.
Twenty-five patients (42 percent) had a confirmed eye stroke based on OCT imaging and follow-up examination. Ten patients were eligible for treatment and nine received treatment with intra-arterial tPA. There was a statistically significant improvement in their visual acuity four weeks after treatment. Researchers noted a dramatic improvement in 66 percent of these patients within 24 hours of treatment, with 56 percent of treated patients maintaining improved vision one month following the procedure. On average, the patients’ vision improved dramatically—from “counts fingers” (but not able to read the eye chart) to 20/100. Most notably, four patients (44 percent of those treated with tPA) improved to 20/40 or better, which constitutes unrestricted driving vision in New York State.
“We reported a novel protocol for the diagnosis of eye strokes that not only can save vision for these patients, but also demonstrates the potential to use remote consultation for time-sensitive ophthalmic emergencies,” says Gareth Lema, MD, PhD, lead author of the study and Vice Chair of Quality, Safety, and Experience at NYEE.
Next steps for the Mount Sinai researchers’ campaign to improve eye stroke outcomes will include expanding the availability of OCT cameras in more Mount Sinai Health System emergency rooms and increasing outreach to the medical community and the general public. The goal is for people to better understand symptoms of eye stroke and the importance of getting immediate medical attention, and recognize the potential for treatment to preserve vision with a timely referral.
“The importance of education among the medical community and the public cannot be stressed enough. Patients with an eye stroke are at risk of also developing a stroke in the brain, and that risk is highest in the first month after diagnosis. If patients get to us in time, we can treat. But even for those who don’t, the systemic work up to identify the source of the stroke might be even more critical,” adds Dr. Lema.
Source: Mount Sinai
More info: A Remote Consult Retinal Artery Occlusion Diagnostic Protocol. Ophthalmology. Published February 13, 2024