Neovascular AMD: Is Telomerase a new Treatment Target?
Researchers determined in mice that telomerase, an enzyme related to cell growth and division, is a culprit in the blood vessel invasion in the back of the eye that causes blurred central vision in neovascular age-related macular degeneration (AMD). Targeting the enzyme with an experimental drug suppressed abnormal vascular growth in the animals’ retina.
Choroidal neovascularization (CNV) is the principal driver of blindness in neovascular age-related macular degeneration (nvAMD).
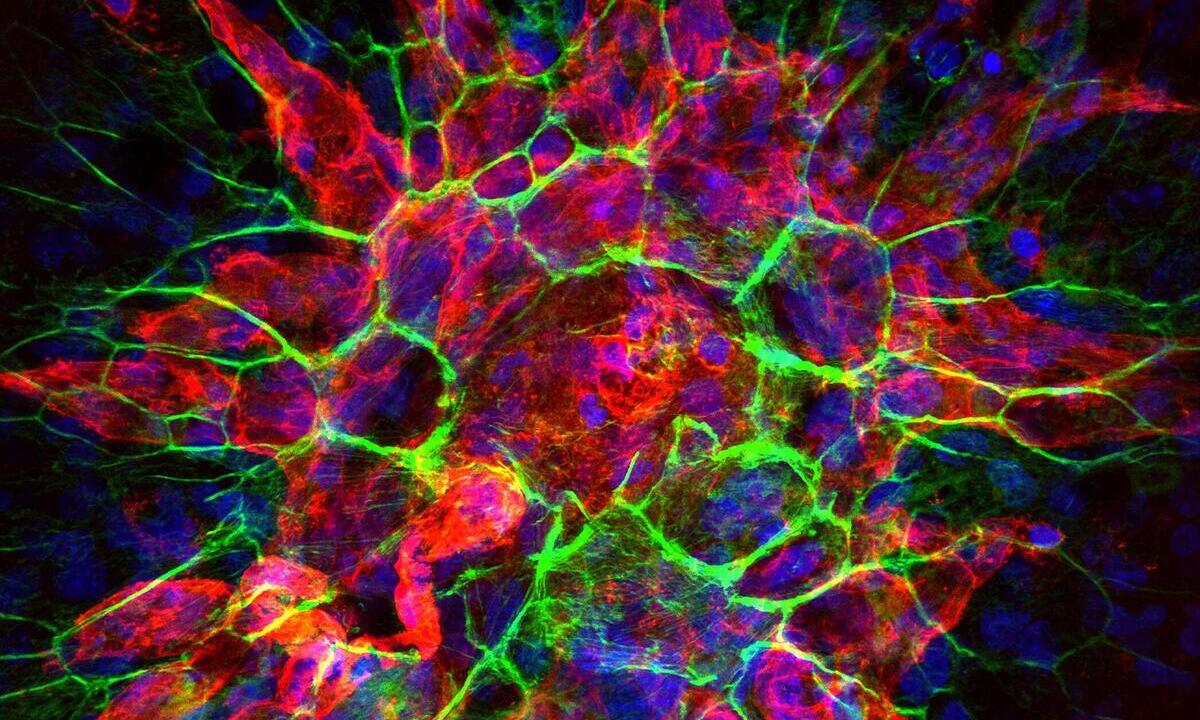
Increased activity of telomerase, has been associated with endothelial cell proliferation, survival, migration, and invasion in the context of tumor angiogenesis. Expanding on this knowledge, we investigated the role of telomerase in the development of CNV in mouse model. We observed increased gene expression and activity of telomerase in mouse CNV.
The only current treatment for neovascular AMD is injection of a medication that blocks the activity of a growth factor protein, called VEGF, which is also known to prompt formation of abnormal blood vessel growth in this condition.
“Anti-VEGF treatment has shortcomings – after two years, about half of people stop responding. And patients can develop scarring under the retina,” said senior study author Nagaraj Kerur, associate professor of ophthalmology and visual sciences in The Ohio State University College of Medicine.
“There is a need for better understanding of the mechanisms behind this problem, which, to me, means newer targets need to be tested.”
The study was published recently in the journal Biochimica et Biophysica Acta – Molecular Basis of Disease.
Increased activity of telomerase, has been associated with endothelial cell proliferation, survival, migration, and invasion in the context of tumor angiogenesis. Previous cancer research has also shown the enzyme can stimulate production of VEGF. Based on those findings, Kerur and colleagues investigated the role of telomerase in the development of CNV in mouse model.
Telomerase has a role in abnormal blood vessel formation
A series of experiments first confirmed telomerase has a role in abnormal blood vessel formation. Researchers found that, compared to control mice, expression, and activity of one of two genes carrying instructions for making telomerase were higher in the eyes of mice in which rapid growth of new blood vessels was induced with a laser.
In addition, the abnormal blood vessel response to laser injury was significantly lower in mice lacking both telomerase genes, “providing genetically clear evidence that telomerase plays a critical role in development of the disease,” Kerur said.
The team then tested the effects of an experimental compound that inhibits telomerase activity. They confirmed that the drug lowered telomerase activity in healthy mice and found that injecting it into the eyes of mice with symptoms mimicking neovascular AMD significantly reduced the abnormal blood vessel invasion.
Telomerase’s job is to rebuild telomeres, which function as protective caps at the end of chromosomes. Telomeres are known to shorten in many types of cells as a consequence of aging, but Kerur said the study suggested localized blocking of telomerase in the eye had no bearing on the enzyme’s telomere-building function.
Curbing abnormal blood vessel growth
The experimental treatment’s effectiveness at curbing abnormal blood vessel growth in mice was similar to the current anti-VEGF treatment, Kerur said. But the researchers made an intriguing finding when testing both drugs at lower doses: Individually, a lower dose did not have much of a therapeutic effect, but a combination of both drugs at lower doses gave the best results of all.
“Possibly, one goal would be using a combination therapy rather than one alone,” Kerur said. “But telomerase inhibition by itself can also be pursued independently, and that is the plan.”
Source: The Ohio State University
Biochimica et Biophysica Acta – Molecular Basis of Disease: Therapeutic targeting of telomerase ameliorates experimental choroidal neovascularization