Glaucoma: New drug delivery method promises long-lasting relief
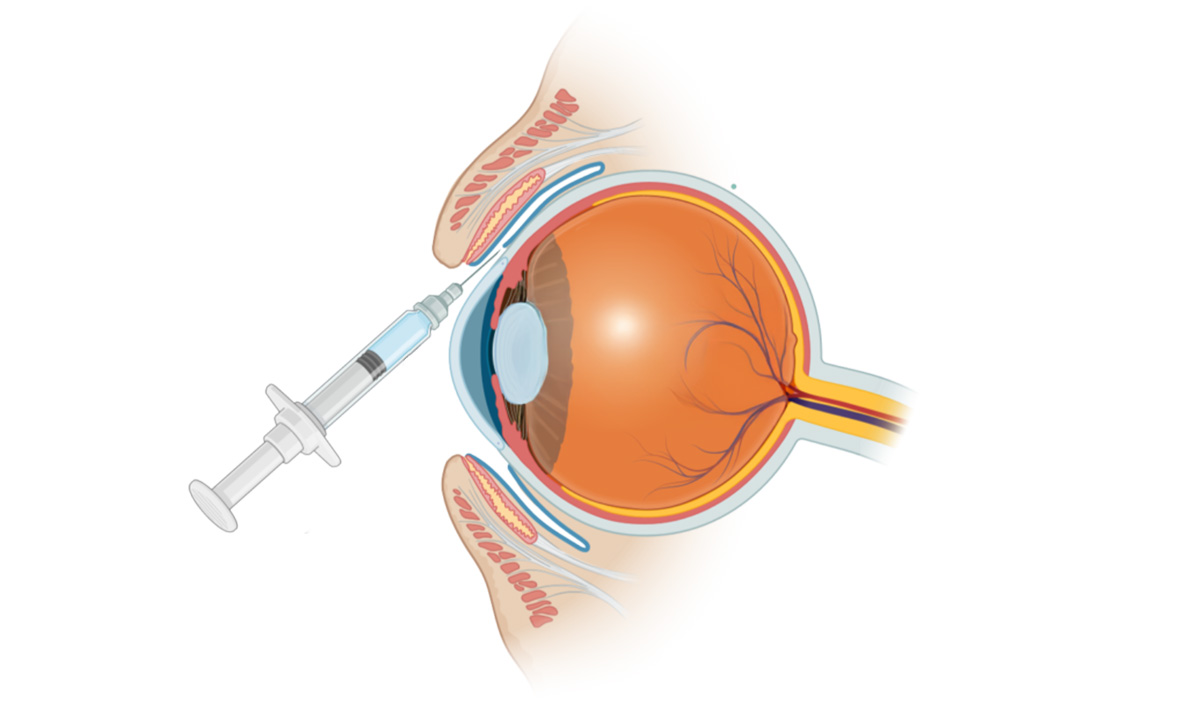
The approach developed by researchers at the University of Toronto could replace daily eye drops with a single injection into the subconjunctival space that lasts nearly two months.
A team led by Molly Shoichet, a professor in the department of chemical engineering and applied chemistry and the Institute of Biomedical Engineering, used colloidal drug aggregates (CDAs) to modify the effects of timolol. CDAs are self-assembled, amorphous, drug-rich nanoparticles.
This new approach, described in a recent paper in the journal Advanced Materials, prolongs the drug’s effect from six hours when it is delivered via an eye drop to up to seven weeks with a single, non-invasive injection into the subconjunctival space of rat eyes.
“Eye drops are the most common treatment for glaucoma, but they come with issues regarding efficacy and patient compliance, especially since the disease is more common in older adults,” says PhD alumnus Mickaël Dang, a postdoctoral fellow in Shoichet’s lab and the first author of the study. “Self-administering drops perfectly can be difficult and their effects are transient, requiring administration on a precise, interval-based schedule.
Timolol prodrug colloids dispersed in a hydrogel
The research team’s new method delivers timolol prodrug colloids dispersed in a hydrogel, demonstrating for the first time that a non-colloid forming drug can be chemically modified into a colloid-forming prodrug.
CDAs are drug molecules that can spontaneously self-assemble into nano-scale particles. Traditionally, they have been seen as a hindrance in drug development research. This is due to CDAs creating false positive and false negative results in enzyme- and cell-based assays, respectively, which are commonly used to screen and characterize drug candidates in the early stages of development.
“We showed that delivery of this colloidal drug aggregate could be dispersed in an in situ-forming hydrogel into the subconjunctival space,” says Shoichet.
Systemic blood concentrations of timolol significantly lower
The intraocular pressure was significantly reduced for at least 49 d with a single subconjunctival injection of timolol-palmitate CDAs compared to 6 h for conventional timolol maleate. The systemic blood concentrations of timolol were significantly lower, even after 6 h, for timolol palmitate CDA-loaded hydrogel versus free timolol maleate, thereby potentially reducing the risk of systemic side effects.
“The colloidal drug enabled the slow release over several weeks leading to a 200-fold increase in efficacy and the hydrogel resulted in the formulation staying in the subconjunctival space after injection. The control – without the hydrogel – mostly leaked out of that space.”
Shoichet’s lab collaborated with Jeremy Sivak, the glaucoma research chair at the Krembil Research Institute, part of the University Health Network, and an associate professor in U of T’s department of ophthalmology and vision science in the Temerty Faculty of Medicine.
Given the success of their preclinical research, the researchers are now working towards optimizing their formulation for ultimate clinical use.
“We envision a future where this non-invasive injection can be administered once every month or two in a medical office,” says Dang, who is also at Synakis, a spinoff biotechnology company founded from research in Shoichet’s lab.
“We invented this novel hydrogel as a vitreous substitute for vitreoretinal surgery, and here we show its versatility to encapsulate and release small molecule drugs.”
“There is a lot of work ahead,” adds Shoichet. “We are focused on the stability and manufacturability of our product while at the same time looking to raise funds to advance it more quickly to the clinic.”
Source: University of Toronto
Reference: Mickael Dang et al, Colloid‐Forming Prodrug‐Hydrogel Composite Prolongs Lower Intraocular Pressure in Rodent Eyes after Subconjunctival Injection, Advanced Materials (2025). DOI: 10.1002/adma.202419306