Study shows promise for retinal-surgery robot
When even the most highly trained surgeons perform procedures on the retina, the stakes are high. Surgeons must account for patients’ breathing, snoring, and eye movements, along with their own involuntary hand tremors, while they work on a layer of cells less than a millimeter thick.
That’s why researchers at the University of Utah’s John A. Moran Eye Center and the John and Marcia Price College of Engineering have collaborated to create a new robotic surgery device that aims to give surgeons “superhuman” hands.
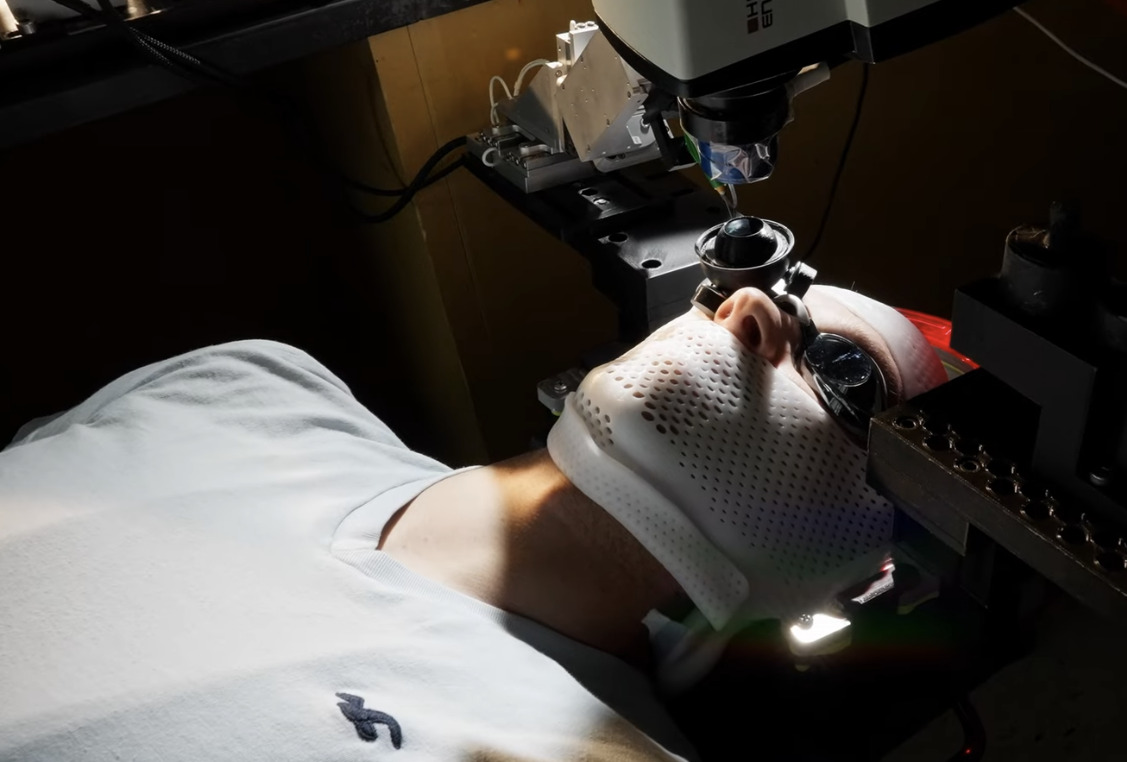
Because the device is not yet approved to operate on human subjects, testing required a human volunteer fitted with special goggles that allowed an animal eye to be mounted just in front of their natural eye.
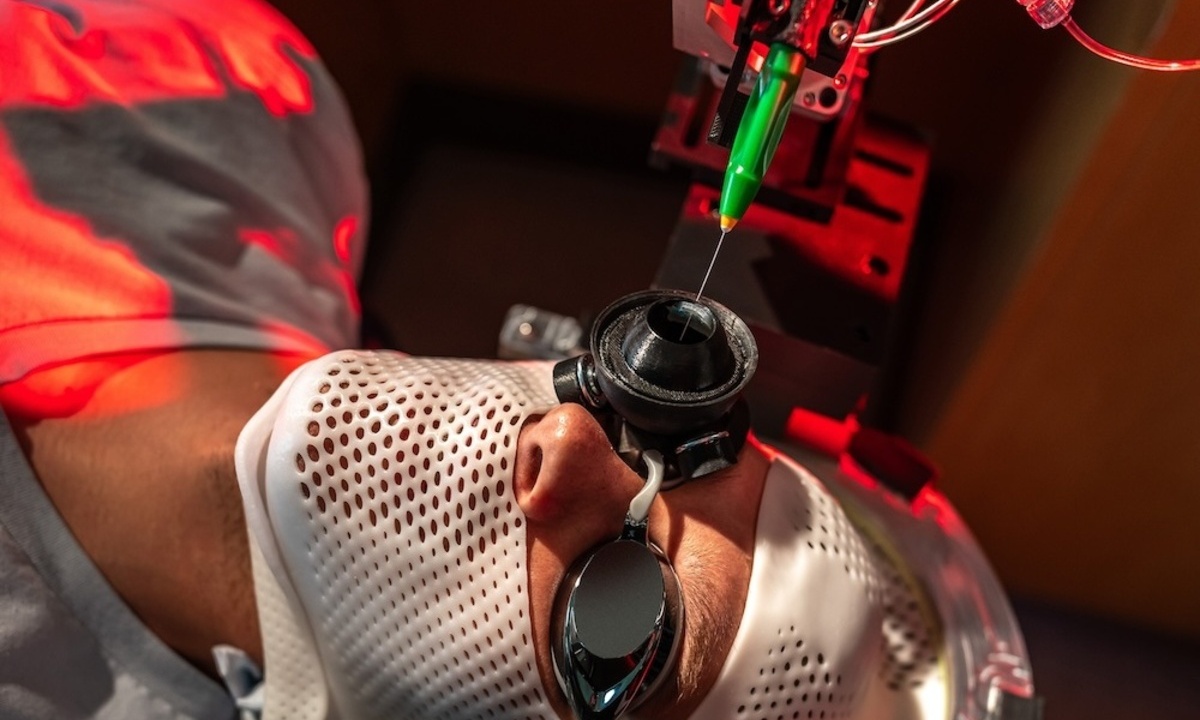
Movements as small as one micrometer
The robot is extremely precise, executing movements as small as one micrometer, or smaller than a single human cell. The robot is also small enough to be mounted directly to the patient’s head using a helmet. Once in place, subtle (and sometimes not-so-subtle) movements of the patient’s head are compensated, keeping the eye quite still from the perspective of the robot. The robot also scales down the surgeon’s movements, measured using a handheld robotic device known as a haptic interface, to the much-smaller surgical site within the eye, compensating for hand tremors along the way.
Video: Research on New Head-Mounted Robotics Device Offers a Glimpse into the Future of Eye Surgery
While still in testing stages, the device aims to improve outcomes for patients and support cutting-edge procedures, including the delivery of gene therapies for inherited retinal diseases.
The researchers successfully tested the robot using enucleated pig eyes, publishing their results in the journal Science Robotics. The study was led by Jake Abbott, a professor in Price Engineering’s Department of Mechanical Engineering, and Moran Eye Center retinal specialist Paul S. Bernstein, MD, PhD. Coauthors include Abbott lab members Nicholas Posselli, PhD, and Zachary Olson, Moran Eye Center retinal specialist Eileen Hwang, MD, PhD, and Aaron Nagiel, MD, PhD, of the University of Southern California’s Keck School of Medicine.
The retina is home to the light-sensitive rod and cone cells that form the basis of vision. Several inherited disorders cause those cells to form incorrectly, leading to vision impairments of ranging severity, but new gene therapy techniques promise to reverse those conditions.
“Treatments for vision disorders are rapidly advancing,” Abbott says. “We need to give surgeons better ability to keep up with them.”
The subretinal target is vanishingly small
The first FDA-approved gene therapy for an inherited retinal disease, for example, requires an injection into the space between the retina and the retinal pigment epithelium. In addition to the complications presented by eye movement and hand tremors, this subretinal target is vanishingly small; the surgeon must introduce the drug between two submillimeter-thin cell layers.
Testing the device required a human volunteer fitted with special goggles that allowed an animal eye to be mounted just in front of their natural eye. This allowed the researchers to test the robot’s ability to compensate for head motion and correct for hand tremors, all while operating on animal tissue.
The experiments demonstrated the success rate when using the surgical robot device to be higher than documented manual rates in some studies.
“The unique feature of this robot, head mounting, may make it possible for patients to have subretinal injections under intravenous (IV) sedation, rather than general anesthesia,” Hwang says. “IV sedation allows for faster recovery, and is safer in some patients. Robots may also allow for more precise delivery of gene therapy medication compared to manual injections for more reproducible, safer treatments.”
As the robot makes its way from the lab to the operating room, its journey will be bolstered by the kind of interdisciplinary collaborations that first brought it to life.
“These collaborations are just wonderful at the University of Utah,” Bernstein says. “When I have ideas, the engineers, the chemists, the physicists, are just a few blocks away.”
Source: University of Utah College of Engineering